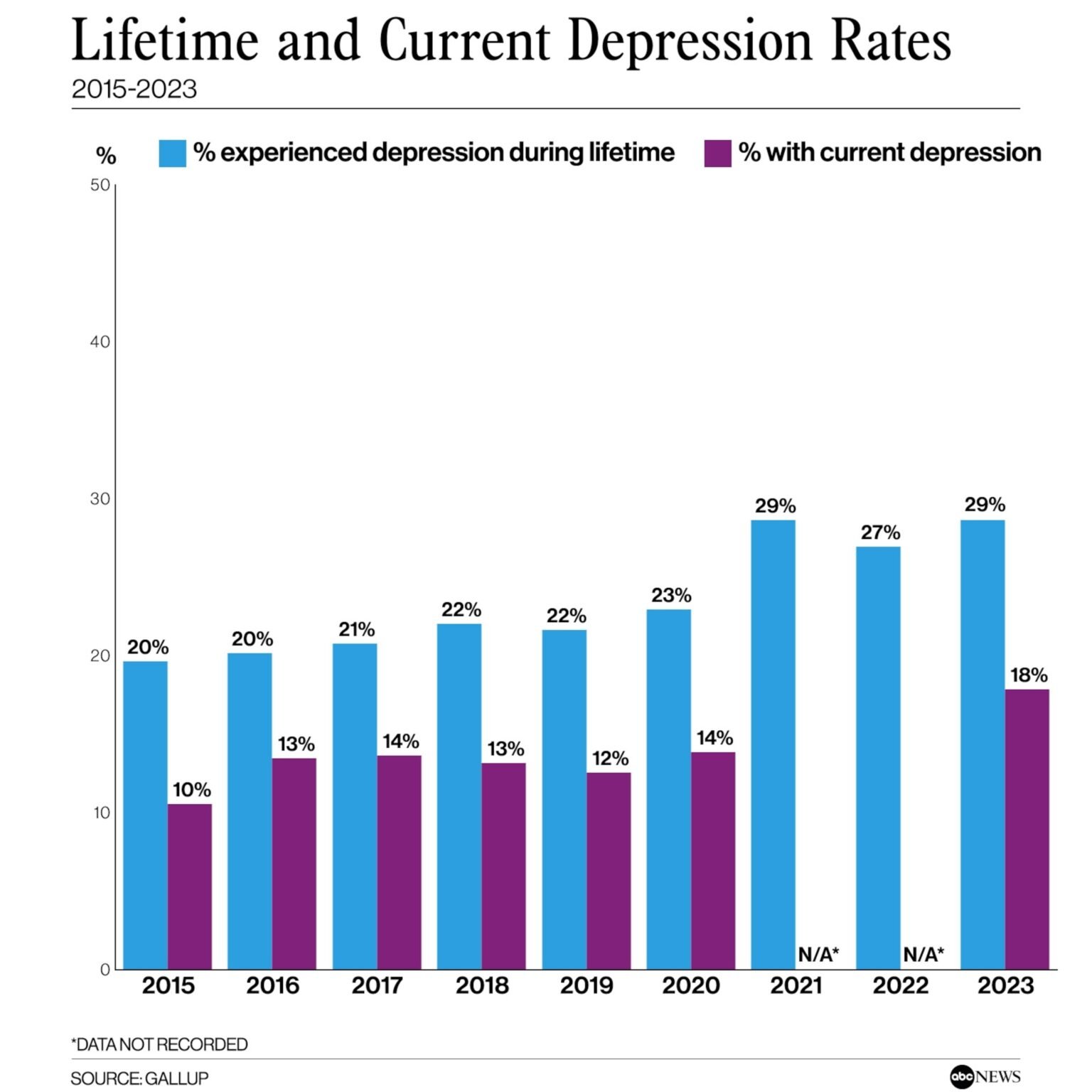
In life, everyone experiences down days or moments of sadness, which is perfectly normal. However, when these feelings persist and significantly affect one’s quality of life, it may be more than just simple sadness – it could be clinical depression. Understanding the difference between ‘feeling blue’ and experiencing clinical depression is crucial for early detection and timely intervention. This article aims to shed light on the complex world of mental health, focusing on how to distinguish between a bad mood and clinical depression.

Understanding Clinical Depression: More Than Just Sadness
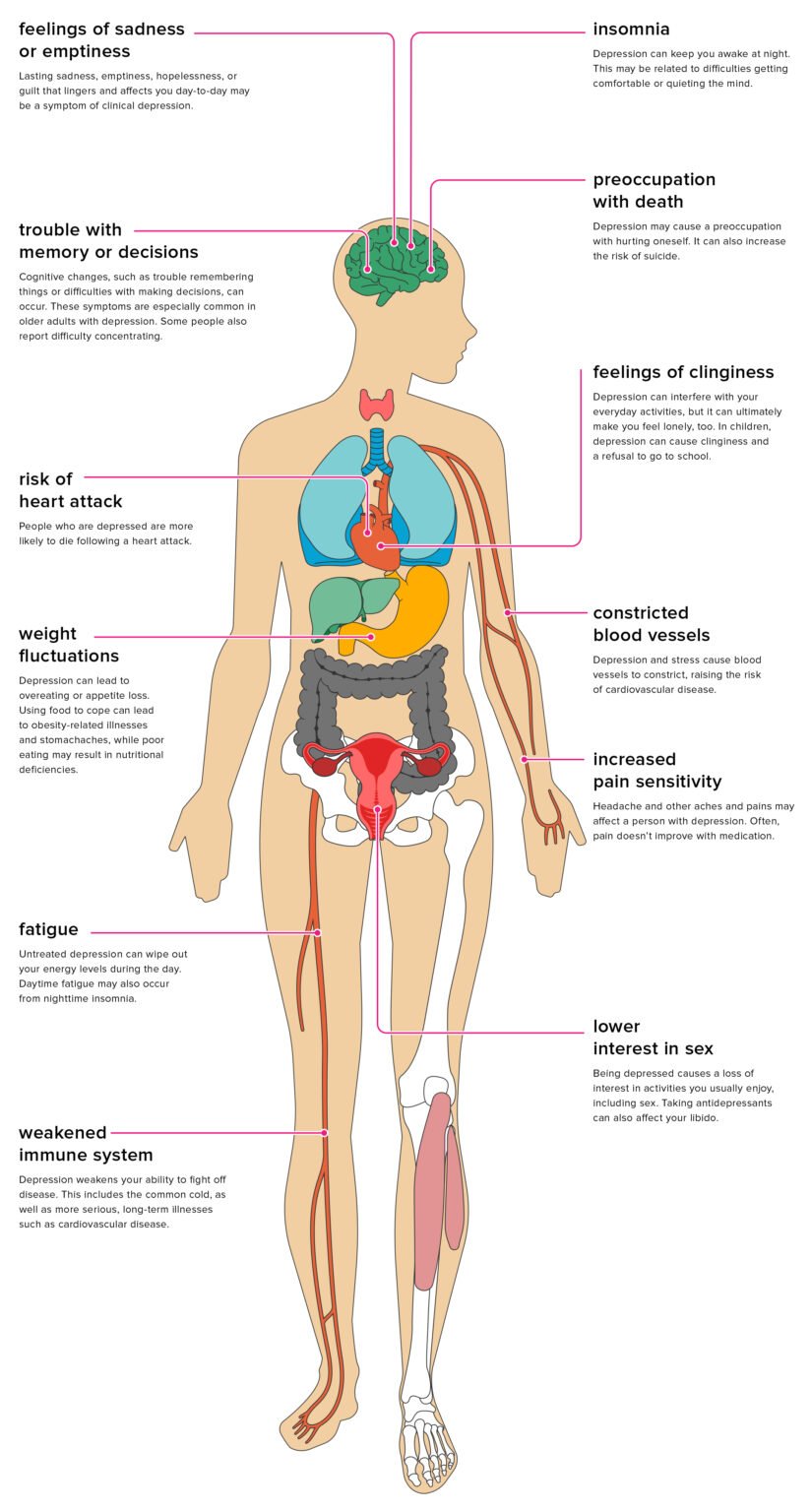
Clinical depression, also known as major depressive disorder, is a common and serious mood disorder that affects an individual’s feelings, thoughts, and behaviors. It causes severe symptoms that can include persistent sadness, loss of interest in activities once enjoyed, changes in appetite, difficulties with sleep, and even thoughts of death or suicide. These symptoms are not fleeting – they persist for at least two weeks and can last much longer, often disrupting work, school, family, and social life.
Clinical depression is not a sign of personal weakness or a condition that can be willed away. It’s a complex interplay of genetic, biological, environmental, and psychological factors. It can affect anyone at any age, but it most often begins in adulthood. Depression is not only limited to feelings of sadness or grief, but it can also manifest as irritability, restlessness, or a seemingly unprovoked anger.
[hostinger-affiliate-table id=”1524″]
Depression isn’t a uniform condition; it exists on a spectrum, with symptoms and experiences varying significantly between individuals. Some people may experience a single episode of major depression, while for others it may recur throughout their lives. Additionally, people with clinical depression might not appear visibly sad or down. This is what makes understanding and diagnosing depression so complex – it doesn’t look the same for everyone.
Spotting the Differences: Bad Mood vs. Clinical Depression
Everyone experiences bad moods or periods of sadness, which can be triggered by life events such as a stressful day at work, a breakup, or the death of a loved one. These feelings of sadness, disappointment, or frustration are normal reactions to life’s ups and downs. However, once these feelings persist beyond a reasonable period of time and start interfering with daily activities and personal relationships, it may be a sign of clinical depression instead of just a bad mood.

A key aspect of distinguishing a bad mood from clinical depression is the duration and impact of the symptoms. In general, symptoms of a bad mood or temporary sadness will dissipate within a few days and will not significantly interfere with daily life. On the other hand, symptoms of clinical depression persist for at least two weeks, and these symptoms are severe enough to disrupt daily activities.
[hostinger-affiliate-table id=”1525″]
Another important difference is the presence of physical symptoms. While a bad mood might not have a substantial physical impact, clinical depression often comes with physical symptoms such as changes in appetite, weight, sleep patterns, and energy levels. Moreover, people with depression often experience feelings of worthlessness, excessive guilt, and recurrent thoughts of death or suicide, which are not typical characteristics of simply being in a bad mood.

Understanding the difference between a bad mood and clinical depression is crucial for early detection and appropriate treatment. Clinical depression is a serious mental health condition that requires professional help, and it should not be mistaken for just feeling down or blue. If you or someone you know is experiencing symptoms of depression, it’s essential to seek help from a healthcare professional. Remember, it’s okay to ask for help – mental health matters just as much as physical health.